How to Manage a Dual Diagnosis
The article is developed in partnership with BetterHelp.
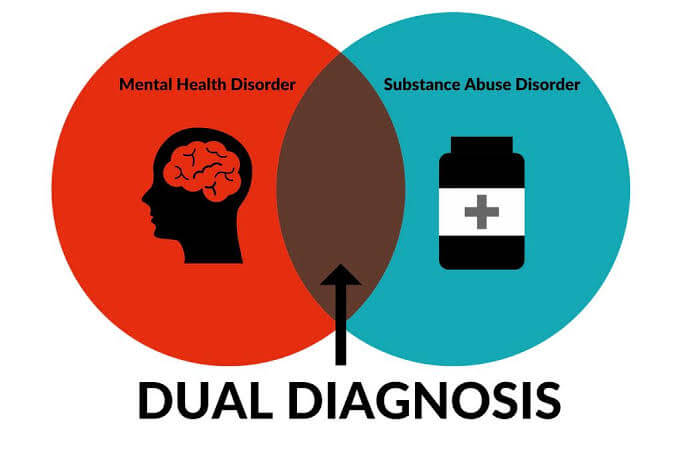
Living with a dual diagnosis – the presence of both a mental health condition and a substance use disorder – can be a challenging journey. It’s important to understand the details of a dual diagnosis, along with its prevalence, symptoms, and potential causes – and most importantly, how to effectively manage this complex condition.
What is a Dual Diagnosis?
Dual diagnosis is the term used to describe a situation where a mental health condition and a substance use disorder, such as alcohol or drug addiction, are present at the same time.
It’s important to note that dual diagnosis isn’t a singular diagnosis, but actually a combination of two separate conditions. Mental health challenges can include depression, anxiety, and others, while substance use disorders involve addiction to alcohol, drugs, or other addictive substances.
How Common is a Dual Diagnosis?
Research shows that dual diagnosis is a fairly common occurrence, affecting roughly 50 percent of people who experience a substance use disorder during their lives.
In 2020, a staggering 17 million U.S. adults experienced co-occurring mental health conditions and substance use disorders.
What are the Symptoms and Potential Causes of a Dual Diagnosis?
The symptoms of dual diagnosis are diverse and depend on the specific combination of mental health and substance use disorders involved. Common symptoms of substance use disorders may include withdrawal from social circles, difficulty concentrating, and engaging in risky behaviors.
Symptoms of mental health conditions may range from extreme mood changes and confusion to thoughts of suicide.
Figuring out which disorder emerges first is complex – and a lot like answering the old chicken-and-egg question. Substance use and mental health conditions share some common risk factors like genetics, stress, and childhood trauma. Mental health challenges may lead some people to self-medicate through substance use, while substance use can alter brain function, increasing the likelihood of developing a mental health disorder.
When it comes to diagnosing the two conditions, overlapping symptoms create difficulty for healthcare professionals. Healthcare providers use comprehensive screening tools – but they also rely heavily on patient honesty to accurately assess the presence of both conditions.
Open communication with your healthcare provider is critical for establishing an effective diagnosis and treatment plan.
How to Manage a Dual Diagnosis
Effective treatment for dual diagnosis involves addressing both the mental health and substance use components at the same time. Behavioral therapy, including cognitive-behavioral therapy and dialectical behavioral therapy, has proven effective in treating co-occurring disorders. Medication, support groups, and in-patient care may also be part of the comprehensive treatment plan tailored to the individual’s needs.
Continued collaboration with healthcare providers and engagement in support groups can be tremendously helpful for sustained recovery. If you’d like to find out more about how group therapy can be especially effective in addressing the conditions involved in a dual diagnosis, you can find out more from the trusted resource BetterHelp.
It’s important to remember that while a dual diagnosis might be challenging, with appropriate and comprehensive treatment, people with dual diagnoses can expect positive outcomes and a much-improved quality of life.
By understanding the interplay between mental health and substance use, seeking accurate diagnosis, and embracing comprehensive treatment strategies, it’s entirely possible to embark on a path toward recovery and a fulfilling life. Dual diagnosis is not a journey anyone has to face alone – reaching out for help is always the first step toward healing.