Beta Blockers| Example, Types, Effect and symptoms
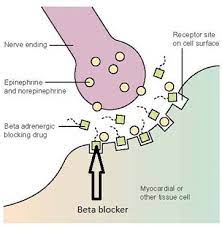
Beta blockers, sometimes called “beta-adrenergic” blocking medications, which stops “norepinephrine” and “epinephrine” “adrenaline” from binding to beta receptors on neurons. Nerves all over the body, as well as the adrenal gland, create norepinephrine and epinephrine. They function as neurotransmitters (chemicals that nerves use to connect with one another) that can be active locally where they are created or throughout the body when released into the bloodstream. The human body has both alpha and beta receptors. Beta receptors are classified into three categories, each of which controls a different function depending on where they are located in the body.
One, beta-1The heart, eye, and kidneys all have beta-1 receptors.
Two, beta-2The lungs, gastrointestinal system, liver, uterus, blood arteries, and skeletal muscle all have beta-2 receptors.
Three, beta-3 Fat cells include beta-3 receptors.
Beta blockers largely block the effects of “norepinephrine” and “epinephrine” by blocking the 1 and 2 receptors. Beta blockers reduce heart rate by blocking the effects of “norepinephrine” and “epinephrine”, subordinate blood pressure by dilation of blood vessels, and may tighten airways by inducing the muscles that edge the airways to contract which is considered an unfavorable side effect.
Examples of Brands and Generic names for beta blockers
- betaxolol “Kerlone”
- timolol ophthalmic solution “Timoptic”
- betaxolol “Betoptic S”
- timolol “Blocadren, discontinued”
- bisoprolol fumarate “Zebeta”
- carteolol Cartrol,
- metoprolol “Lopressor, Toprol XL”
- carvedilol “Coreg”
- esmolol “Brevibloc
- labetalol “Trandate Norm dyne”
- propranolol “Hemangeol, Inderal LA, Inderal XL, InnoPran XL”
Common Examples of generic and brand names available for beta blockers in the US are: acebutolol (Sectral), atenolol (Tenormin), bisoprolol (Zebeta), metoprolol (Lopressor, Lopressor LA, Toprol XL), nadolol (Corgard), timolol (Blocadren).
What are the side effects of beta blockers?
Common side effect of beta blockers are:
- It gives a timid effect of Diarrhea
- It causes Stomach cramps
- Vomiting
- Nausea
Other significant side effects include:
- Rash
- Disorientation
- Insomnia
- Muscle cramps
- Blurred vision
- Hair loss
- Weakness
- Fatigue
As an extension of their beneficial effect, they slow heart rate and reduce blood pressure, but they may cause adverse effects such as heart failure or heart block in patients with heart problems.
- Central nervous system (CNS) effects of beta-blockers are:
- Headache
- Dizziness
- Depression
- Nightmares
- Hallucinations
- Confusion
- Other significant effect of Beta-blockers:
- In asthmatics, beta blockers that inhibit 2 receptors may produce shortness of breath.
- Sexual dysfunction is possible with this medicine, as it is with other drugs used to treat high blood pressure.
- In patients with diabetes, beta blockers can cause low or high blood glucose and hide the symptoms of low blood glucose (hypoglycemia).
- Beta blockers are a class of medications that inhibit beta-adrenergic chemicals like adrenaline (epinephrine), a crucial agent in the autonomic (involuntary) nervous system’s “sympathetic” nervous system and heart muscle activation. Beta blockers reduce stress on the heart by blocking the action of the involuntary nervous system on the heart.
- Irregular cardiac rhythms, chest pain, heart attack, hypertension, migraine headaches, social phobias, tremors, and glaucoma are all treated with beta blockers.
- If you’re taking diabetes medicine, beta blockers might cause nausea, vomiting, abdominal cramps, diarrhea, and weight gain (type 1 and type 2). Other major side effects and adverse consequences of this medicine class include blurred vision, sleeplessness, hair loss, disorientation, and CNS depression.
Which drugs and supplements interact with beta blockers?
- In diabetics on insulin or other diabetic drugs, beta blockers may prolong “hypoglycemia” (low blood sugar) and hide “hypoglycemia” symptoms.
- When clonidine (Catapres) is used with a beta blocker, or when clonidine or a beta blocker is withdrawn after their concurrent usage, dangerous blood pressure rises can occur. When clonidine or a beta blocker are taken simultaneously, blood pressure should be continuously monitored after beginning or withdrawal. • Phenobarbital and related drugs may enhance the breakdown of propanolol (Inderal) or metoprolol (Inderal) and lower blood levels (Lopressor, Toprol XL). This may reduce the beta blocker’s effectiveness.
- Taking propranolol (Inderal) or pindolol (Visken) together with thioridazine (Mellaril) or chlorpromazine (Thorazine) can cause low blood pressure (hypotension) and irregular cardiac rhythms because the medications interfere with each other’s excretion, resulting in higher levels of the drugs.
- Aspirin and other nonsteroidal anti-inflammatory medicines “NSAIDs” for pain and inflammation
Beta blockers are used to prevent, treat, or relieve symptoms in persons who suffer from the following conditions:
- Beta and alpha-1 receptors are blocked by the drugs labetalol (Normodyne, Trandate) and carvedilol (Coreg). The dilating action of labetalol and carvedilol is enhanced when alpha receptors are blocked.
- Beta blockers may prevent indicators of low blood sugar, such as a rapid heartbeat, in diabetics. If you have diabetes and are taking a beta blocker, it’s critical to monitor your blood sugar on a frequent basis.
- Beta blockers aren’t usually prescribed to people with asthma because there’s a risk that they’ll induce severe attacks.
Beta blockers can have an impact on “cholesterol” and “triglyceride” levels as well. They can cause a little increase in triglycerides, a form of fat in the blood, and a small drop in HDL cholesterol, or good cholesterol. These modifications are frequently only transient.You should not stop using a beta blocker suddenly because it may increase your chance of a heart attack or other cardiovascular condition.